Bronchiectasis is a chronic respiratory condition characterized by the permanent dilation and damage of the bronchi, the tubes responsible for carrying air in and out of the lungs. This condition can lead to frequent infections, difficulty breathing, and a reduced quality of life if left unmanaged. Understanding the most common cause of bronchiectasis is vital for prevention, early detection, and effective treatment.
In this article, we’ll explore the primary cause of bronchiectasis, delve into other contributing factors, and discuss strategies for managing and preventing the condition. Our focus will be to provide clear, accessible information to enhance understanding and awareness.
Contents
Understanding Bronchiectasis
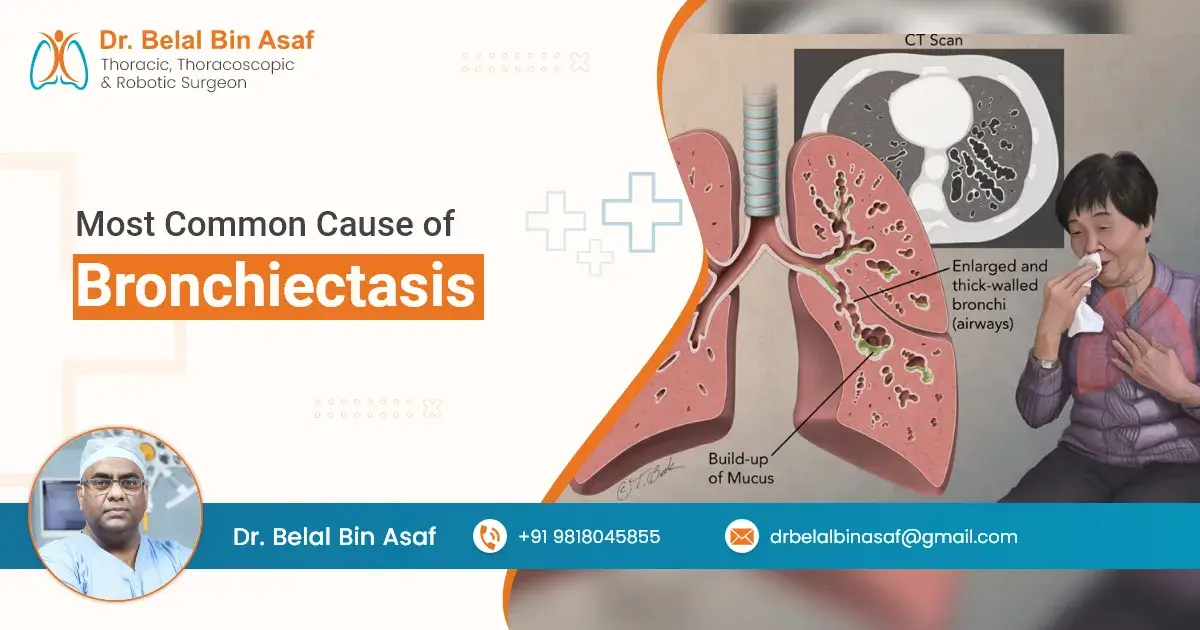
To grasp the causes, it’s essential to understand the underlying pathology of bronchiectasis. The bronchi are lined with cilia, tiny hair-like structures that help clear mucus and debris from the airways. In bronchiectasis, these airways become abnormally widened, leading to impaired ciliary function, mucus buildup, and an increased risk of infections. Over time, this creates a vicious cycle of inflammation and further airway damage.
The Most Common Cause: Post-Infectious Damage
Among the various causes of bronchiectasis, post-infectious damage is the most common. Severe respiratory infections, particularly during childhood, can lead to structural damage in the bronchi. Infections such as pneumonia, tuberculosis, and pertussis (whooping cough) have historically been significant contributors.














 +91-9818045855
+91-9818045855