Lung cancer poses a serious threat to respiratory health, triggering a range of physiological disruptions that can significantly impair breathing and overall lung function. Gaining a clear understanding of these effects is essential for patients, caregivers, and healthcare professionals to effectively manage symptoms and enhance quality of life. This in-depth look explores the various ways lung cancer interferes with normal respiratory processes, including blocked airways, fluid buildup, and reduced oxygen delivery.
Contents
- 1 Airway Obstruction and Impaired Ventilation
- 2 Pleural Effusion: Fluid Accumulation Around the Lungs
- 3 Hypoxemia: Decreased Oxygen Levels in the Blood
- 4 Other Respiratory Symptoms and Complications
- 5 Impact on Quality of Life and Psychological Well-being
- 6 Diagnostic Approaches and Monitoring
- 7 Treatment Strategies
- 8 Conclusion
Airway Obstruction and Impaired Ventilation
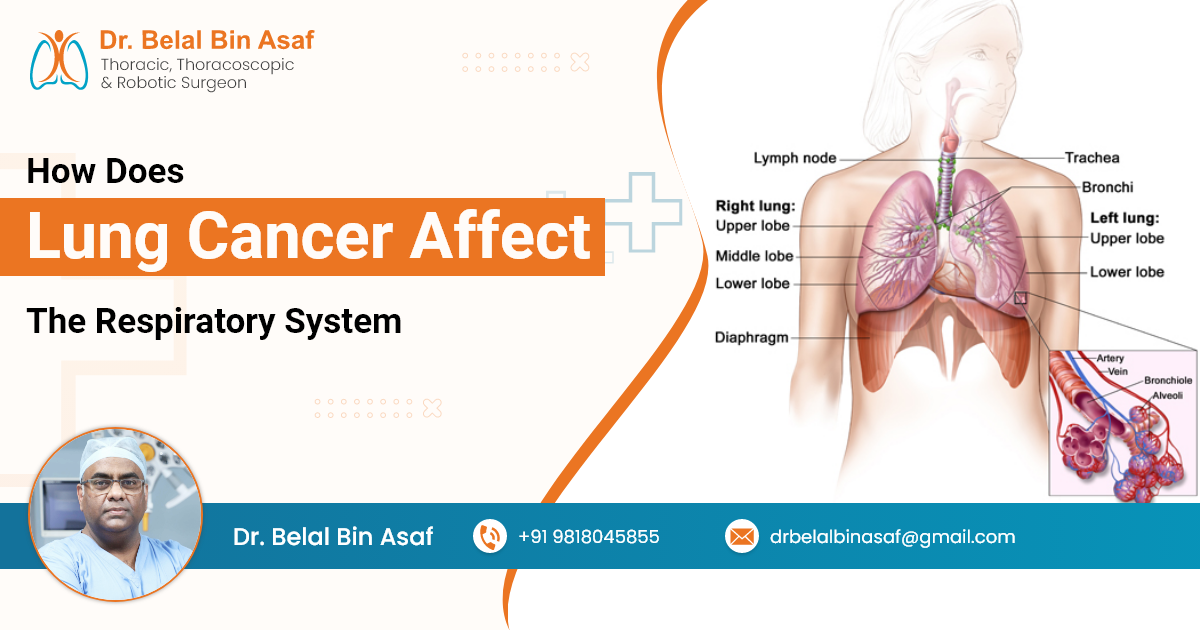
Lung cancer often originates in the bronchi or bronchioles, the primary air passages leading to the lungs. As the tumor grows, it can partially or completely obstruct these airways, leading to several respiratory issues:
- Dyspnea (Shortness of Breath): Blocked airways reduce airflow, making breathing difficult and causing a sensation of breathlessness.
- Persistent Cough: Tumors can irritate the airways, leading to chronic coughing, which may be dry or produce sputum.
- Atelectasis: Partial collapse of lung tissue occurs when an airway is obstructed, reducing lung volume and impaired gas exchange.
- Post-obstructive Pneumonia: Stagnant air and mucus in blocked airways can lead to infections, further complicating respiratory function.
These symptoms are particularly common in central tumors, which are located near the center of the chest, affecting major air passages.
Pleural Effusion: Fluid Accumulation Around the Lungs
Pleural effusion refers to the accumulation of excess fluid between the pleura—the double-layered membrane surrounding the lungs and lining the chest cavity. Lung cancer can cause pleural effusion through several mechanisms:














 +91-9818045855
+91-9818045855