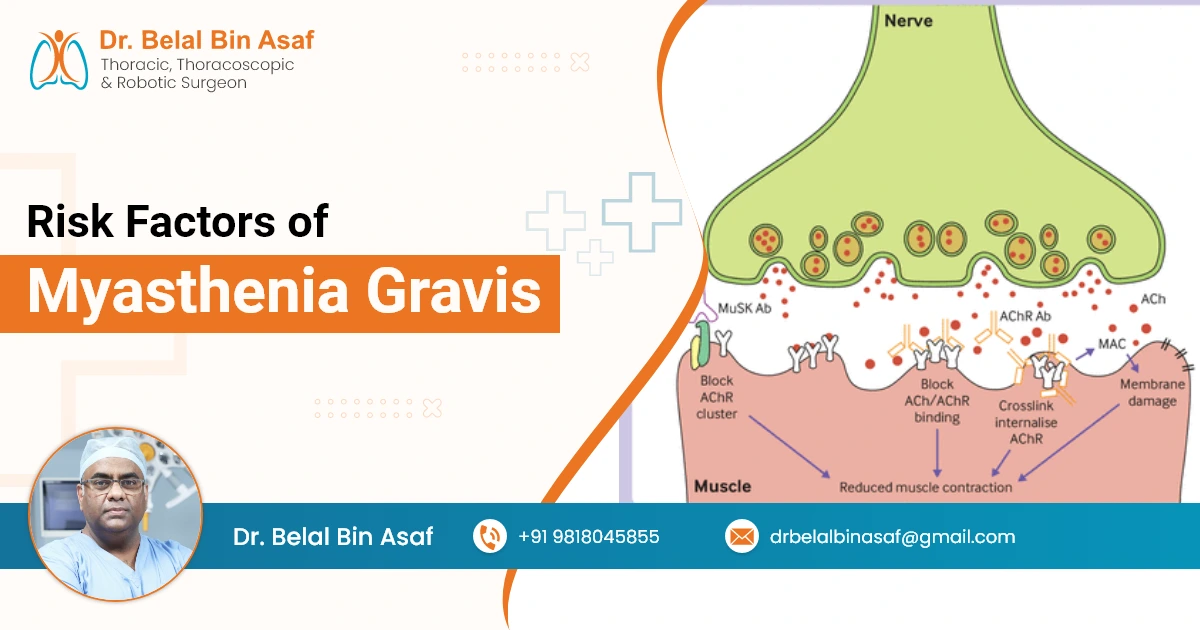
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder that causes weakness in the skeletal muscles, which are responsible for activities such as breathing, moving the arms and legs, and maintaining posture. In MG, the body’s immune system mistakenly attacks the communication between nerves and muscles, specifically the acetylcholine receptors at the neuromuscular junction. This disruption results in muscle fatigue and weakness that typically worsens with activity and improves with rest.
While the precise cause of MG remains unclear, researchers have identified several risk factors that can increase the likelihood of developing the condition. Understanding these factors is crucial for early diagnosis, effective management, and support for those living with this rare but manageable disorder.
Contents
1. Gender and Age
Myasthenia gravis does not affect all individuals equally. There is a distinct pattern in age and gender distribution:
- Women under the age of 50 are more frequently diagnosed with MG.
- Men over the age of 60 also show a higher incidence of the condition.
This age and gender discrepancy suggests that hormonal and immunological factors may influence susceptibility. For instance, fluctuations in estrogen and other sex hormones could potentially affect the immune system’s activity in women during their reproductive years.














 +91-9818045855
+91-9818045855